Welcome to our Patient Guide to everything you need to know about Medicare and Cataract Surgery. In this article, we’ll answer common questions such as:
- Does Medicare Cover Cataract Surgery?
- What Services Does Medicare Cover For Cataract Surgery?
- Which Medicare Plans Cover Cataract Surgery?
- How much Does Medicare Cover For Cataract Surgery
- What Doesn’t Medicare Cover For Cataract Surgery
This article will prepare you to discuss insurance with your doctor and their surgical counselors. Let’s get started!
Does Medicare Cover Cataract Surgery?
This is one of the most common questions asked by patients with early symptoms of cataracts or patients who are in the age range for cataracts,
Good news… The answer is ‘Yes’!
However… That’s just the short answer… There are additional things to consider because while Medicare typically covers at least some of the cost of cataract surgery, it often doesn’t cover all of it. This commonly results in patients having some out-of-pocket expenses.
Cataract surgery has advanced tremendously over the last few decades. As technology has advanced, making surgery safer and achieving better vision outcomes than ever before, medical insurance plans, such as Medicare have not extended their coverage for these new technologies.
So while it is true that Medicare does cover basic manual cataract surgery for any type of cataracts, in the next section we’ll discuss the details of exactly what it covers, and what it doesn’t cover.

What Services Does Medicare Cover For Cataract Surgery?
Medicare covers a basic version of cataract surgery, performed by hand, with a basic lens implant, that is not customized to your eyes. It also covers 90 days of routine follow-up care. Some of the other things it typically covers:
- Pre-operative eye exam to diagnose your cataracts
- Limited pre-operative measurements for basic lens implants
- Anesthesia during surgery
- Removal of cataract
- Facility fee
- Basic (monofocal) lens implant
- Contribution to one pair of prescription eyeglasses after surgery
- 90 days of follow-up care for issues related to the procedure
What Should Patients Expect After Basic Cataract Surgery With Medicare?
After basic cataract surgery, patients should expect to need bifocals and trifocals for their best vision.
This is because Medicare is a type of “medical insurance”.
Medical insurance is different from vision insurance plans. Medical insurance draws a line saying that removal of the cataract and replacement with a basic lens implant fulfill their responsibility as a medical insurance provider, and if a patient would like to be free from glasses, either with a modern lens implant, laser vision correction, or glasses, then that is the patient’s responsibility.
Out-Of-Pocket Expenses with Medicare
To achieve better vision after surgery, many Medicare patients have the option of adding non-covered services to their cataract surgery at an out-of-pocket expense.
Practices use different names to describe these non-covered services or refractive packages.
If you are considering a modern lens implant or laser cataract surgery, it’s important to remember that Medicare will still be paying its portion of the surgery. Any out-of-pocket payment is made in addition to what Medicare covers.
In the next sections, let’s get into specific examples of the services you’ll have the option of choosing for your cataract surgery, and discuss them in the context of Medicare.
Which Medicare Plans Cover Cataract Surgery?
There are different Medicare Plans. These plans include the following:
- Original Medicare
- Medigap (Medicare Supplemental Insurance)
- Medicare Advantage
Let’s go over the differences, and what each of these covers for cataract surgery.
Original Medicare
This includes Medicare Part A and Medicare Part B. Part A covers hospital insurance, skilled nursing facilities, nursing home care, hospice, and home health care. Part B covers non-hospital medical care, including medically necessary services and preventative services.
Medicare Part B applies to most cataract surgery performed in an outpatient setting. However, there are some patients who have their surgery in the hospital, in which case Part A would apply.
How much you may pay differs whether your surgery is performed in a hospital versus in the outpatient setting, since the reimbursements for services under Part A and Part B are different.
Medigap or Medicare Supplemental Insurance
Supplemental insurance plans help cover the out-of-pocket expenses relating to Medicare-covered services. For example, Medicare Part B covers 80% of the approved Medicare charges (once your annual deductible is met). Medicare Supplemental plans help cover the remaining 20% that is left over.
These supplemental plans can vary significantly. Review with your supplemental insurance plan your premium, deductible, co-pays, and how much you should expect to pay anytime you have a medical procedure.
There are many different plans. Your surgeon’s office will likely know the details of the more common plans in your area.
Medicare Advantage
Medicare Advantage plans, which are referred to as “Part C”, are provided by private commercial insurance companies, however, they are required to follow rules set by Medicare.
These Medicare Advantage plans may be HMO or PPO-based or fee-for-service. They may also include prescription drug plans, which can be referred to as Part D.
While these plans are required to follow certain rules set forth by Medicare, there are differences between the various plans that private insurance companies offer.
When it comes to cataract surgery, the basic parts of cataract surgery are covered, but they will be subject to deductible and co-pay rules set forth in your plan.
Discuss the details with your insurance provider if you have questions.
How Much Does Medicare Cover For Cataract Surgery?
There are several fees associated with cataract surgery that Medicare covers. These are the surgical center facility fee, the surgeon fee, and the anesthesia fee (in some cases).
These fees can differ based on region and whether your surgery is performed in a hospital, ambulatory surgical center, or office-based surgical center.
If Your Procedure is in an Ambulatory Surgical Center (ASC)
As of 2022, most cataract surgery in the United States is performed in an ambulatory surgical center. According to Medicare’s procedure lookup tool, the national average for the doctor and facility fee for routine cataract surgery (code 66984) are:
- Doctor Fee: $544
- Facility Fee: $1,062
- Total Fee: $1,606
If Medicare pays 80% of this amount, then it will cover $1,284. The remaining 20% is the responsibility of the patient, which amounts to $320.
If Your Procedure is Performed in a Hospital
If your cataract surgery is performed in a hospital, the doctor’s fee remains the same. However, the facility fee increases to reflect the higher expenses of operating a hospital.
- Doctor Fee: $544
- Facility Fee: $2,120
- Total Fee: $2,664
In this situation, Medicare will still cover 80%, which amounts to $2,131. The patient will be responsible for $532 per eye. Please note that these numbers are from 2022.
Does Medicare Cover Complications After Surgery?
Cataract surgery is one of the safest procedures. But no medical procedure is perfect, and every patient is different. Complications can occur after cataract surgery that may result in additional care.
Some patients go into surgery with complicated medical and ocular histories. They’ve had previous trauma or surgery on their eyes, and their cataracts can be advanced. It is natural for the risk of complications to be higher in these cases.
So what happens if you have a complication that requires additional medical care?… Does Medicare cover it?
Medicare covers 90 days of follow-up care related to cataract surgery. If something happens within the 90-day period that is determined to be unrelated to the surgery, then the medical care for these services may be covered but will be billed separately, meaning that you may be required to pay additional fees.
What Doesn’t Medicare Cover For Cataract Surgery?
Modern cataract surgery gives most patients the option of using lens implants and lasers to achieve a higher quality of vision after their procedure. Medicare does not cover the following list of services. (In insurance lingo, these are called “non-covered services”, which means that patients are required to pay out-of-pocket if they’d like these services.)
- Astigmatism Correction
- Presbyopia Management with Multifocal Implants
- Advanced-Technology Lens Implants
- Multifocal Lens Implants
- Toric Lens Implants
- Extended Depth of Focus Lens Implants
- Certain Imaging/Diagnostic Technology That Assists in Better Vision Outcomes
- Laser Cataract Surgery
Let’s review each of these non-covered services, discuss what they are, why it may be right for you, and explain Medicare’s coverage, or lack thereof.
Does Medicare Pay For Cataract Surgery With Astigmatism Correction?
The answer to this may surprise you. Astigmatism correction is a basic and fundamental part of vision correction. However, Medicare does not cover cataract surgery with astigmatism correction.
As a result, patients who only have the basic lens implant are missing out on a great benefit of modern cataract surgery. Specifically, they are missing out on freedom from bifocals and trifocals.
Whenever any type of surgery is considered, patients and their doctors should discuss the risks, benefits, and alternatives of the available treatment options. Both doctors and patients seek to maximize the benefits of surgery while reducing the risks.
Astigmatism correction, such as during cataract surgery with toric lens implants, can achieve an improved postoperative vision, without adding significant risk to the procedure. By choosing astigmatism correction at the time of surgery, most patients are improving the risk-benefit ratio in their favor.
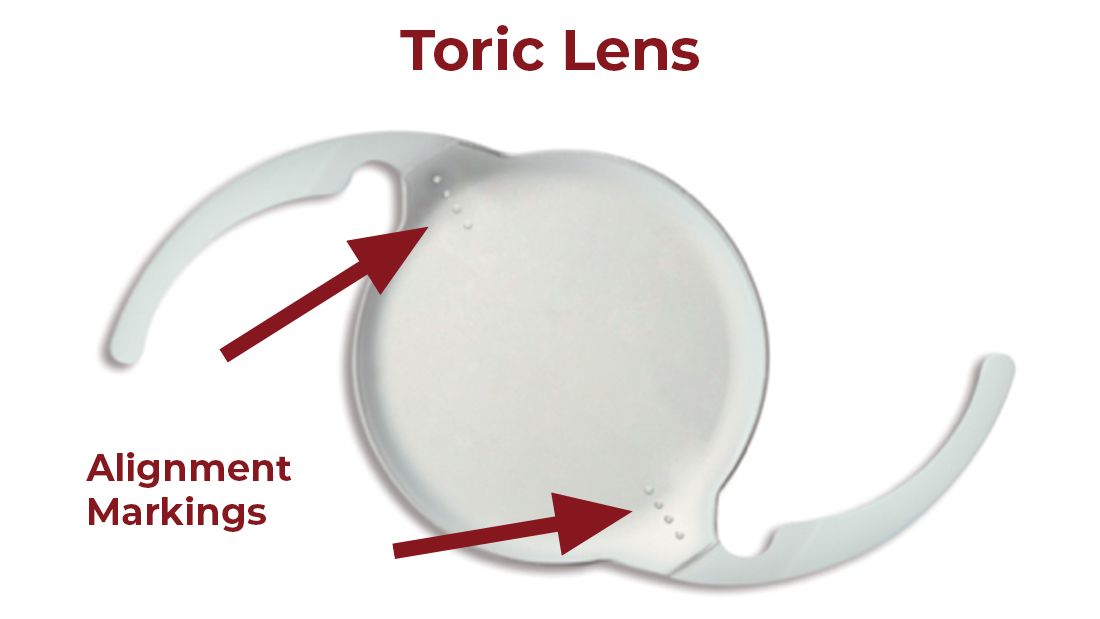
*Note the special dotted markings on the lens used to align it to fix astigmatism.
When considering the out-of-pocket cost of astigmatism correction, it’s important to also consider the cost of bifocals and trifocals. Typically, after cataract surgery, one’s glasses prescription does not change. So if you achieve freedom from glasses and contact lenses, it is typically for the rest of your life.
However, if you do not have your astigmatism managed, and require bifocals or trifocals, these glasses can be expensive. Typically, most people replace their glasses every 2-3 years. A “no-line bifocal”, also known as a “progressive bifocal”, can be very expensive, and after factoring in the replacement cost of a new pair every 2-3 years, it doesn’t take long before choosing astigmatism management becomes a better long term financial decision for many patients.
Does Medicare Pay For Multifocal Lens Implants?
If you’ve read the previous section about astigmatism correction, then this one will be very similar.
Just as Medicare and other medical insurance companies do not consider “astigmatism management” to be a covered service, similarly, they do not consider “presbyopia management” to be a covered service.
Ultimately, presbyopia is the diagnosis that multifocal implants treat.
Presbyopia is the name given to the condition that naturally occurs with aging in which the natural lens stiffens, losing its ability to provide a range of vision without bifocals or reading glasses.
Monofocal lens implants are similarly stiff and do not have the advanced optics required to provide patients with the range of vision necessary to be free from reading glasses.
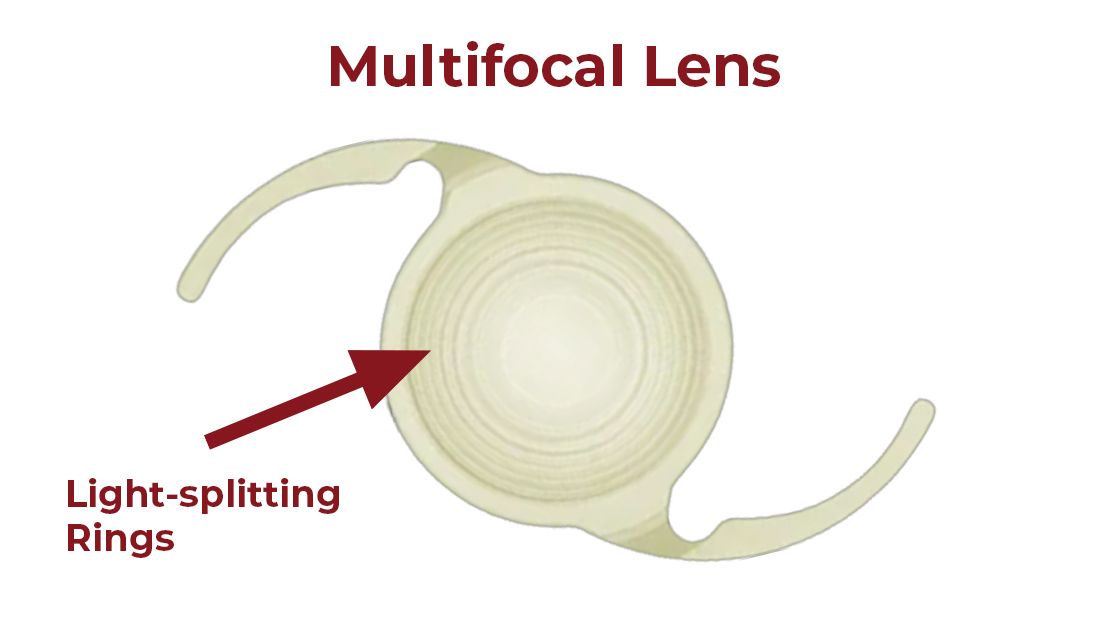
*Note the special rings used to split light resulting in multifocal optics.
To address presbyopia at the time of your cataract surgery, there are a few options, one of which is implanting a multifocal lens implant. Common multifocal implants include the PanOptix implant and Synergy intraocular lens implant.
The goal of multifocal lens implants is to achieve freedom from glasses for both distance and near vision activities.
Just like with astigmatism management, Medicare and other medical insurance do not cover the cost of these modern lens implants. They will still cover the other aspects of the surgery, but patients should expect an out-of-pocket expense if they select a multifocal implant.
Does Medicare Cover EDOF lens implants?
Extended depth of focus (EDOF) implants also help patients achieve increased freedom from reading glasses. While their optics may be different from multifocal implants, Medicare treats them the same. Medicare does not cover them. An example of an extended depth of focus IOL is the Vivity lens implant.
Does Medicare Cover the Crystalens implant?
The Crystalens intraocular lens implant also corrects presbyopia. The Crystalens implant works differently from diffractive MFIOLs and EDOF lenses. However, it similarly reduces dependence on reading glasses. Once again, Medicare treats Crystalens the same and does not cover it.
Does Medicare Cover the Light Adjustable Lens Implant?
No. Similar to other advanced technology lens implants, Medicare does not cover the light adjustable lens implant. This is because the light-adjustable lens corrects astigmatism, which is a non-covered service. The goal of the light-adjustable lens is to achieve some amount of freedom from glasses.
Does Medicare Cover Laser Cataract Surgery?
You may be noticing a theme here as we continue discussing modern technology used in cataract surgery.
Just like the technology used to fix astigmatism and presbyopia, laser cataract surgery is not covered by medical insurance.
Complex computer and imaging systems guide laser cataract systems. The first step of a laser cataract procedure is taking high-resolution images of the eye. After obtaining these images, computer software identifies the structures and landmarks for the laser treatment. Under the guidance of these computer systems, the laser is then applied, performing steps of the procedure with precision and consistency that the human hand can’t match. It is common to use laser cataract systems to correct astigmatism as well.

Medical insurance does not cover the advanced imaging associated with laser surgery, or any associated astigmatism management or presbyopia management.
Patients should expect to pay an out-of-pocket fee for laser cataract surgery.
What Type of Lens Does Medicare Cover For Cataract Surgery?
Medicare covers a basic monofocal lens implant without the management of astigmatism or presbyopia.
That means toric lens implants, or monofocal implants with corneal astigmatism treatment, are not covered.
Patients who receive this type of lens implant without the management of astigmatism should expect to need glasses for all distances after cataract surgery. This is commonly achieved with a bifocal or trifocal pair of glasses.
Summary
We hope this article was able to give you a great overview of what Medicare covers and does not cover for cataract surgery. Medicare and other medical insurance plans do not cover several modern cataract technologies. Hopefully, this article prepares you for this before you set foot in a surgeon’s office. However, it’s important to remember in these situations that Medicare typically does still cover much of it, including pre-operative & post-operative office visits, anesthesia fees, surgical center fees, and the basic parts of the procedure, such as removing the cataract. However, like so many areas of medicine, technology has made cataract surgery better, and to have these benefits you should expect to pay an out-of-pocket fee.
Be sure to browse our Resources for more information about cataract surgery, and to find a cataract surgeon near you.